Published on MedEdgeMEA on May 31th
Introduction: A New Frontier for Liver Transplantation
Precision medicine has transformed fields like oncology and cardiology, but liver transplantation has been left behind. Despite being a domain where decisions often mean life or death, the field still relies on outdated clinical scoring systems. But this is changing. The tools of precision diagnostics – genomics and artificial intelligence (AI) – are here, and they will reshape how we select, treat, and follow liver transplant patients.
The Limitations of Traditional Scoring Systems
The MELD score, introduced more than two decades ago to prioritize liver disease patients for transplantation, was a step forward in bringing objectivity to organ allocation. But it’s, at best, a blunt instrument. MELD is built on a narrow set of lab values and doesn’t reflect the biological diversity of liver disease, particularly in complex cases like hepatocellular carcinoma (HCC) or acute decompensation. It can’t account for tumor genomics, disease heterogeneity, or the molecular drivers that are now known to shape patient outcomes. Poor outcomes are the consequence. Moreover, after transplantation, patient management remains largely standardized, with little room for personalisation based on individual risk profiles or molecular characteristics.
Precision Diagnostics: Transforming Patient Selection
But that’s beginning to change, driven by the medical community’s commitment to advancing the field. In Europe, for example, the LEOPARD consortium, led by clinicians and researchers, is building large prospective liver transplant cohorts with the clear goal of creating new allocation models that combine clinical and genomic data. Similarly, groups like EF CLIF are developing predictive tools for acute-on-chronic liver failure that integrate advanced clinical and molecular insights. These efforts mark a move toward decisions that are not only fairer but also biologically smarter.
Innovations in Liver Cancer: Towards Personalized Transplantation
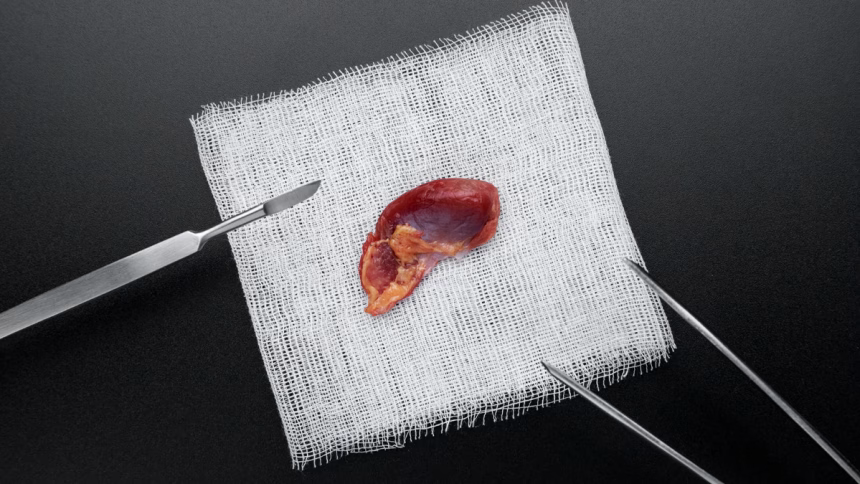
In liver cancer, precision tools are already emerging. AI-based models are being developed to more accurately predict long-term survival after transplantation, while genomics-enabled approaches are providing improved prognostic insights. HepatoPredict, for example, leverages tumor biopsy biomarker data and machine learning to help identify which patients are most likely to benefit from a transplant. This kind of individualized risk assessment not only enhances patient selection but also paves the way for more tailored post-transplant strategies, for example flagging patients who require closer surveillance or informing targeted risk-reduction interventions.
Post-Transplant Monitoring: The Promise of Liquid Biopsy and AI
Post-transplant monitoring is also evolving. There is a growing trend toward the development of liquid biopsy technologies for earlier and less invasive detection of complications after liver transplantation. For example, HepatoDetect analyzes methylation patterns in circulating tumor DNA and is being explored as a tool to catch signs of recurrence earlier, although further validation for minimal residual disease is still needed. This kind of minimally invasive surveillance could give clinicians a head start, helping them intervene before a full relapse occurs. Several other platforms are moving in the same direction, bringing AI and genomics into the post-transplant setting in ways we couldn’t have imagined a decade ago. And in an era of Transplant Oncology, new tools will bring new hope. In addition, liquid biopsies are also being developed and validated for the early detection of organ rejection, allowing clinicians to intervene at the optimal moment for maximal benefit.
Global Perspectives: The Middle East as a Leader in Precision Transplantation
The Middle East, and the Gulf region in particular, is well positioned to lead this shift. With significant investments in digital health and an expanding transplant infrastructure, there is a unique opportunity to bypass legacy systems and build precision into transplantation from the ground up. For example, Saudi Arabia is pioneering robotic living donor liver transplantation – KFSHRC in Riyadh performed the world’s first fully robotic living donor and recipient liver transplants, including the first fully robotic left lobe procedure, dramatically advancing precision, safety, and recovery in liver surgery. Recent high-profile Kuwait-UAE organ sharing partnerships – such as the urgent cross-border liver transplant that saved a patient’s life in Abu Dhabi (1) – demonstrate the region’s growing capacity for collaborative, life-saving transplantation efforts. Collaboration, data-sharing, and openness to innovation will be key.
Looking Ahead: Challenges and Opportunities
We’re entering a new era. The question is no longer whether genomics and AI will change liver transplantation: it’s how soon, and who will lead the way. Of course, challenges remain: integrating complex data into clinical workflows, ensuring equitable access, and navigating regulatory pathways will require determination and collaboration. Yet these are not insurmountable barriers; they are the next frontiers for innovators and leaders in the field. If we get it right, we won’t just match patients and organs: we’ll maximize the life-saving potential of liver transplantation, offering every patient the best possible chance for a healthy future. That’s the future this field deserves. Now.
